There is currently no cure for COPD. There are two main goals of treatment. The first is to help control your symptoms and improve exercise tolerance, so you can carry on with your daily activities and improve your overall health status. The second goal is to reduce the risk of complications, by slowing down the disease progression, and by preventing and treating COPD flare-ups.
Your healthcare provider will work with you to review your symptoms and to adjust your treatment plan accordingly. If you want to keep an overview of how well your symptoms are under control, you may want to keep a symptom diary at home.
Even though this symptom diary hasn’t been formally studied in research, it may still help you remember how you felt at different times and make it easier to discuss your COPD with your doctor.
Examples of these documents can be downloaded here for personal use (permission to distribute for personal use only!).

If you haven’t already, then the most essential step in your treatment plan for COPD will be to quit smoking. Although the damage to your lungs that has already been done can’t be reversed, quitting smoking will prevent further loss of lung function. No matter how long you have had COPD, quitting smoking can help slow progression of the disease. Your symptoms, like breathlessness, coughing, and phlegm will improve and you will be less likely to experience COPD flare-ups. Find out more about quitting smoking in our Lifestyle and Prevention module.

Most COPD medicines are taken using an inhaler. These small, hand-held devices deliver the medicine directly into the lungs, so it doesn’t need to travel through the bloodstream to reach its target.
Some medicines are taken using a nebuliser, which is a machine that turns liquid medicine into a fine mist that you can breathe in through a mask or a mouthpiece. Nebulizers are mainly used in hospitals during severe flare-ups to deliver higher doses of medicine. In some cases, they can also be used at home for people with more advanced COPD, especially if inhalers are no longer effective or too difficult to use.
Bronchodilators are medicines to help open up your airways. They are considered the cornerstone of treatment for patients with COPD. Bronchodilators are categorized based on the duration of effect.
Short-acting bronchodilators work within a few minutes to relax the muscles in your airways and relieve your symptoms. They are prescribed for use ‘as needed’ when symptoms flare-up.
There are two types of short-acting bronchodilators:
You might be prescribed a combination of SABA and SAMA, depending on the severity and frequency of your symptoms.
If you experience breathlessness on a daily basis, your doctor will probably prescribe a long-acting bronchodilator. These medicines help relax and open up the muscles in your airways, making it easier to breathe. They act more slowly than short-acting bronchodilators, but their effects last much longer, usually between 12 and 24 hours. When taken regularly, they help keep your airways open and support your breathing throughout the day.
There are two types of long-acting bronchodilators:
Many people with COPD who experience breathlessness use a combination of two long-acting medicines: a LABA and a LAMA. The combination can be prescribed as two separate inhalers or as a single combination inhaler, which is often more convenient and more effective than multiple inhalers, but sometimes a bit more expensive. Expected side effects are those of the separate medicines.
Steroids, also called corticosteroids, are medicines that help reduce inflammation. When inhaled, they act directly in the lungs to decrease swelling and irritation. Not everyone with COPD needs inhaled steroids (ICS). These inhalers are usually prescribed for people who have frequent COPD flare-ups or higher levels of a certain type of white blood cells called ‘eosinophils’. They are also recommended for people who have both COPD and asthma. Inhaled steroids only work properly when used on a regular basis, so it is important to use them as prescribed. It is also important to know that this treatment mainly helps reduce the number of flare-ups, but it has less effect on day-to-day symptoms compared with other inhalers such as LAMA or LABA.
In terms of expected side effects, it is important to know that inhaled steroids work locally in the airways, at the site of the inflammation. Hence, only a little enters the blood stream, leading to few side effects. Oral thrush (a yeast infection in the mouth) is the most common side effect, which you can help prevent by rinsing and gargling with water after using your inhaler. Hoarseness or a sore throat can also occur but are less common. In people with more severe COPD, there may be a slightly higher risk of developing a chest infection called pneumonia. If your doctor prescribes an inhaled steroid, it will usually be as part of a combination inhaler that also includes a bronchodilator, sometimes even a triple combination with a LABA, LAMA, and ICS. If you are ever concerned about side effects, talk to your doctor.
Ensifentrine is a relatively new treatment for COPD that helps both to reduce inflammation in the lungs and to open up the airways (a bronchodilator effect). It is taken by inhalation and can help improve breathing and reduce the number of COPD flare-ups. It is currently only available in the United States.
Taking your medicines the right way is just as important as taking them regularly. For your inhaled treatment to work properly, it needs to reach the lungs. Take your time to watch an inhaler technique video that matches your inhaler device and review any materials your doctor has provided about using your medicines correctly. Remember to bring your inhalers to each doctor’s appointment so that your technique can be checked regularly. Your pharmacist can also support you in making sure you’re using your inhalers correctly.

Steroids are medicines that help reduce inflammation. Oral steroids – which are taken by mouth – are used for short-term treatment of COPD flare-ups. Long-term use of oral steroids is not advised, as they only help for a short time and can cause more harm than benefit if used regularly. During a short course of oral steroids, you might experience side effects such as increased appetite, difficulty sleeping, or mood changes like irritability or anxiety. When taken regularly or over a longer period of time, oral steroids can also lead to other side effects, including weight gain, osteoporosis, or diabetes.
Oral steroids are sometimes prescribed as part of a so-called ‘rescue-pack’. This is a set of medications you keep at home to use if you experience a COPD flare-up. You should only start the medicines in your rescue pack in accordance with the instructions in your COPD action plan. After using your rescue pack, it is important to get in touch with your doctor. This way, they can check your recovery, review your COPD action plan if needed, and renew your prescriptions.
Mucolytics (for example: carbocysteine or N-acetylcysteine) are medicines that help reduce cough and thin phlegm, which makes it easier to cough up. It is sometimes prescribed as an additional treatment to help prevent COPD flare-ups.
Antibiotics are medicines used to treat chest infections caused by bacteria. Signs of a chest infection are a change in the colour of your phlegm, increased coughing, and being more breathless than usual. You may even develop a fever (body temperature of 38°C/100.4°F or more). Antibiotics are sometimes prescribed as part of a so-called ‘rescue-pack’. This is a set of medications you keep at home to use if you experience a COPD flare-up. You should only start the medicines in your rescue pack in accordance with the instructions in your COPD action plan. After using your rescue pack, it is important to get in touch with your doctor. This way, they can check your recovery, review your COPD action plan if needed, and renew your prescriptions.
Some people with COPD have frequent flare-ups. In these cases, your doctor may propose to add regular antibiotics (such as azithromycin) to your treatment plan. This treatment may help reduce how often COPD flare-ups occur. This treatment is only prescribed and monitored by a COPD specialist.
When you’re prescribed antibiotics, it is important to take them exactly as directed by your healthcare provider. Side effects can vary depending on the type of antibiotic, but the most common ones include diarrhoea and nausea (feeling sick).
Roflumilast is a tablet that reduces the risk of COPD flare-ups. Availability may differ from country to country. Roflumilast may be prescribed for people with chronic bronchitis who have severe or very severe COPD and experience frequent flare-ups. It is used as an add-on treatment, meaning you’ll keep taking your regular COPD medications as well. Side effects include nausea (feeling sick), diarrhoea or weight loss. This medication can cause mood changes in some people such as feeling agitated or depressed. If you or people in your environment notice any changes in your mood, tell your doctor right away.
Theophylline tablets are sometimes used to help relieve shortness of breath, but they are generally less effective and have more side effects than other COPD treatments. As a result, they are less commonly prescribed today. However, in some countries where access to inhalers is limited or costly, theophylline remains more widely used.
For some patients with more severe cases of COPD that also have higher levels of eosinophils (type of white blood cells), the COPD specialist might consider adding biologics to the treatment plan. This is a type of medication that is provided by an injection. Biologics reduce the frequency of flare-ups and improve lung function overall.
The use of biologic treatments in COPD is still relatively new compared with their use in conditions like asthma. However, some biologics have been shown in clinical studies to help reduce the number of flare-ups. At this time, they have not been shown to slow down the overall progression of the disease.
Availability and reimbursement policies differ from country to country. While effective, this treatment can be expensive and it is used in addition to other COPD treatment, including inhalers. So it is often considered when other options are no longer sufficient.
How to self-administer a biologic?
When starting treatment with biologics, your healthcare provider will train you to give yourself a dose via injection. After practicing a few times at the hospital, you will usually be able to do the injections by yourself at home (like insulin injections for diabetes). Since a proper technique is essential for the medicine to work and to ensure you get the full dose, we have created videos to assist you with the correct technique whenever you need it. There are two types of injections: (i) via a prefilled pen or (ii) via a prefilled syringe. Instructions depend on the device you use.
For some people with severe COPD, additional treatments beyond inhalers and medications may be considered to help improve breathing. These include surgical and non-surgical options that target the most damaged areas of the lungs.
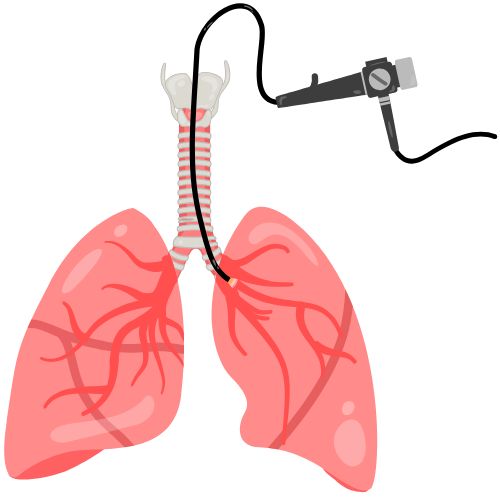
Endoscopic lung volume reduction (ELVR) is a non-surgical procedure used to treat people with severe emphysema. It can achieve similar benefits to traditional surgery but without removing lung tissue. During the procedure, performed under general anesthesia, a bronchoscope (a thin, flexible tube with a light and camera) is used to place small one-way valves into selected airways. These valves allow trapped air to escape from the most damaged parts of the lung, causing them to deflate and shrink. This helps the healthier parts of the lung to expand and function more effectively. Endoscopic lung volume reduction can be an alternative for carefully selected patients who are not suitable candidates for traditional surgery.

Surgery may be an option for some people with severe COPD. When regular COPD treatments are no longer sufficient, your healthcare provider might suggest lung surgery to help improve your breathing.
The two main types of surgery in the context of COPD are:
This surgery involves removing the most damaged parts of the lungs. It is a treatment option for people with severe emphysema. It allows the remaining healthier parts of the lung to expand more fully and work more efficiently. Your healthcare provider may order additional tests to determine whether this type of surgery could be of benefit for you. Not everyone is a suitable candidate. For some people, the risks of surgery may outweigh the benefits.
This involves replacing a damaged lung with a healthy lung from an organ donor. When successful, the transplantation can significantly improve your breathing, quality of life, and the expected course of the disease. However, it is a major operation which – like all operations – carries certain risks. After the transplant, you will need to take medicines to prevent your body from rejecting the donor lung(s). This treatment is only suitable for carefully selected patients with advanced COPD.
If your COPD causes you to have a low level of oxygen in your blood, your healthcare provider may suggest oxygen therapy started at home. This oxygen is provided to you through a mask or through nasal tubes. They are hooked-up to an oxygen tank or an oxygen concentrator machine. Supplemental oxygen is only beneficial to people with low levels of oxygen in the blood. It is important to know that oxygen therapy is not a treatment for breathlessness — the main symptom of COPD. Breathlessness happens because it is harder for you to move air in and out of your lungs, not necessarily because your blood oxygen levels are low.
Oxygen therapy is categorized based on when its being used:
It is important not to smoke when using oxygen. This is because oxygen is a highly flammable gas and if you light a cigarette in close proximity, it could cause a fire.
Depending on how your healthcare system is organized, your GP or respiratory specialist may refer you to a pulmonary rehabilitation programme. This programme is designed for people living with long-term lung conditions who find that breathing problems affect their daily life. It is a structured course of lung physiotherapy, usually offered in group sessions but tailored to your individual needs. Pulmonary rehabilitation is often multidisciplinary, meaning it also involves other specialists such as a dietitian, psychologist, and occupational therapist.
The course focuses on the following topics:
- Exercises to increase your overall fitness, which will make you feel stronger and more energized
- Specific breathing exercises that you can use in times of increased breathlessness
- General information regarding your condition, so that you know more about it and feel empowered
Pulmonary rehabilitation has proven to be beneficial for patients with COPD. It improves your ability to exercise, enhances your quality of life, and it reduces the frequency of COPD flare-ups. Pulmonary rehabilitation is beneficial for most people with COPD. Even if you have severe breathlessness, you might still benefit from the rehabilitation programme.

Although it can be tempting to look for other ways to manage your cough or breathlessness, there is very limited scientific research to support the use of over-the-counter medicines in people with COPD. That is also why their use is not proposed in international guidelines on the treatment of COPD. While you might feel inclined to try cough suppressants (antitussives) or over-the-counter expectorants (medicines to help thin and loosen phlegm), their benefit in COPD is unclear. If you’re thinking about trying any alternative or complementary treatments, always talk to your healthcare provider first to make sure they are safe and suitable for you.
The fact that you're already taking the time to learn more about COPD is a big step forward—well done! Understanding your condition and knowing your treatment options can really help you feel more in control of your condition and your overall health.
Following below are a few tips to help self-manage your condition:
This website does not provide medical advice.
The information, including but not limited to, text, graphics, images, and other material contained on this website is for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis, or treatment and/or medical treatment of a qualified physician or healthcare provider. EUFOREA is not a medical organisation and cannot provide specific medical advice to patients via the Internet and/or E-mail. All patients are encouraged to direct their specific questions to their personal physicians. EUFOREA presents this information to patients so that patients can understand and participate in their own medical care. EUFOREA strongly emphasises that the information contained on this website is not a substitute for thorough evaluation and treatment by a qualified healthcare provider.
© 2025 - EUFOREA - All rights reserved. All content on this portal, such as text, graphics, logos and images, is the property of EUFOREA. They may not be reproduced, copied, published, stored, modified or used in any form, online or offline, without prior written permission of EUFOREA.