
Quitting smoking is the single most powerful thing you can do to take control of your COPD.
Why quitting smoking is one of the best things you can do for your lungs:
That said, we know that quitting smoking is challenging and many people had to go through multiple attempts in order to finally quit for good. The fact that you’re taking the time to read this and even consider quitting is already a big step forward. Even if you’re not ready to quit today, it is helpful to start thinking about when might be the right time for you in the near future.
Talk to your healthcare provider to learn more about stop-smoking programmes in your area, prescription medicines that can support you, and nicotine replacement therapies you could try. You might also find it helpful to connect with others who are going through the same process by joining a support group.
Involving your family and friends can make a big difference too. They can encourage you and support you when things get tough. Finally, try to avoid being around smokers or smoke — not just to reduce temptation, but also because any kind of smoke (including second-hand smoke or smoke from wood fires) can make your COPD symptoms worse.

A healthy lifestyle benefits everyone, but it is especially important when you have COPD.
Eating nutritious foods helps you stay strong. Think of food as fuel for your muscles. Because your lungs have to work harder to breathe, your body uses more energy. This means you may need more calories or protein to keep your muscles working well. You may also need more calcium- and vitamin D-rich foods to keep your bones strong.
When your body is well-nourished, it is also better at fighting infections, which can help lower your risk of flare-ups or hospital visits.
Maintaining a healthy weight is equally important for two key reasons:
Some people with COPD lose weight without meaning to. This can happen for different reasons. Eating may make you feel short of breath, or preparing meals might feel too tiring. Food may also taste different because of mucus you cough up. Sometimes, side effects like nausea or vomiting can make eating harder.
Carrying extra weight can make breathing more difficult, add strain on your lungs and makes obstructive sleep apnea (OSA), a condition that often occurs alongside COPD, more likely.
Tips and tricks on how to eat enough:
Check this excellent resource to learn more about specific nutritional recommendations for people with COPD.
If you need support with healthy eating or your weight, your healthcare provider might be able to refer you to a dietitian. You may also see a dietician as part of a pulmonary rehabilitation programme. If necessary, your provider might recommend taking vitamins or nutritional supplements to meet your nutritional needs.

The amount of exercise that you can tolerate is specific to your individual circumstances. You might become slightly breathless during exercise, but you should not strain yourself too much.
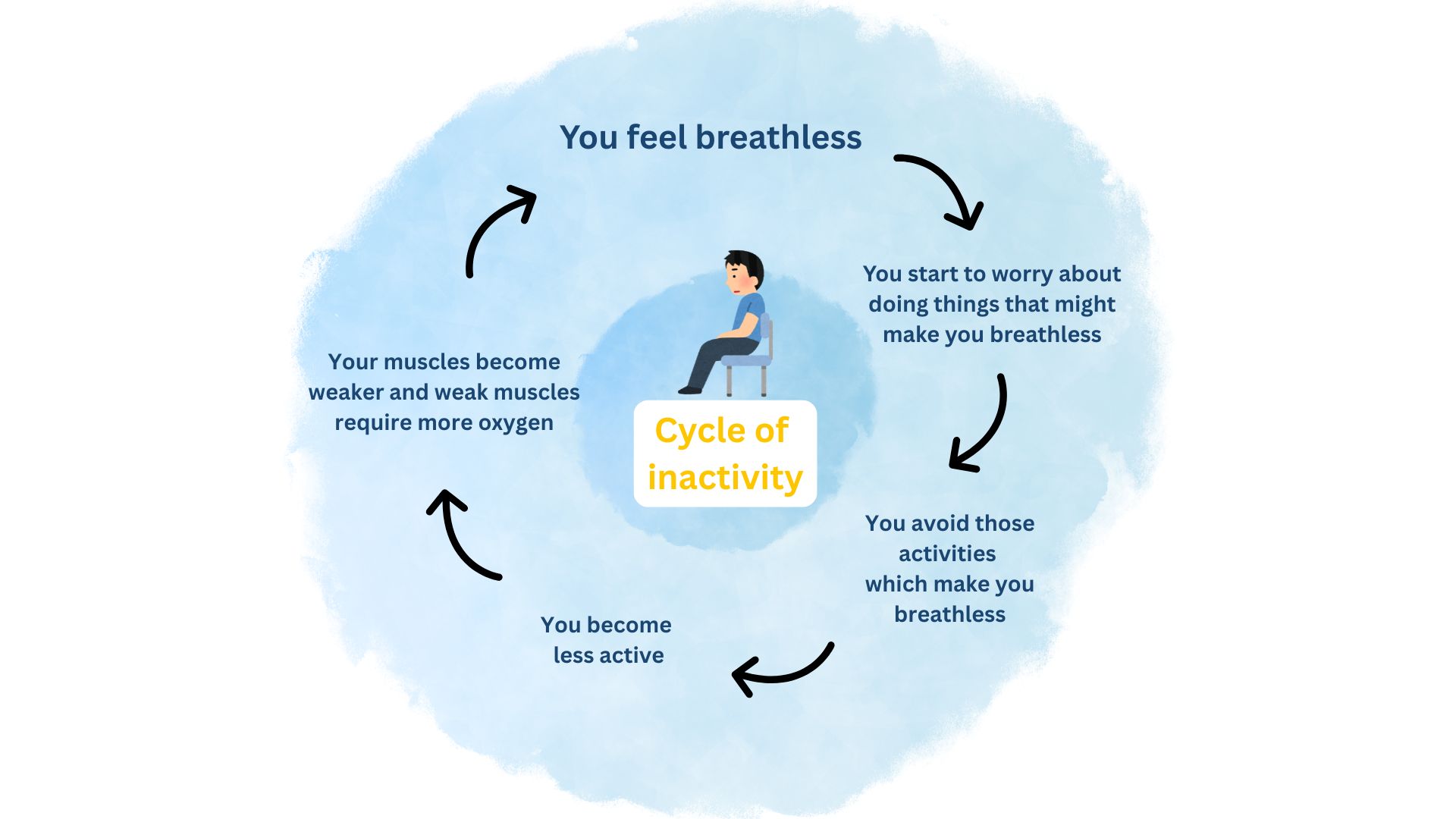
You might feel worried or anxious about exercising, because you’re afraid of getting breathless. This can cause you to avoid physical activity, which in time leads to the loss of muscles strength. Weaker muscles require more oxygen, which in turn can lead to more breathlessness. This is often referred to as the cycle of inactivity. That’s why staying active is so important when you have COPD. Regular physical activity helps improve your overall strength, endurance, and strengthens your breathing muscles, making it easier to manage your symptoms and enjoy a better quality of life.
The amount of exercise you can handle depends on your own health and fitness level. It is normal to feel a bit breathless when you exercise, but you should avoid pushing yourself too hard. Talk to your healthcare provider about which activities are best for you. You may be advised to participate in a pulmonary rehabilitation programme, which is a specialized physiotherapy programme that includes both exercise and education on the condition.

Nowadays, travelling by airplane is accessible to many people. Nonetheless, air travel comes with its own challenges for people with COPD. Although flying with COPD is possible, careful preparation may be needed for safety and comfort
If you are planning a trip by airplane, it is a good idea to discuss this with your healthcare provider. You might be referred for “fit-to-fly” test, also called a Hypoxic Challenge Test (HCT) or High Altitude Simulation Test (HAST). The level of oxygen onboard of an airplane is lower than the level on the ground. HAST measures how well you can cope with less oxygen in the air. It can give an indication for your need for on-board oxygen therapy. If you’re already on oxygen therapy, you’ll need to either take your own materials with you on board or arrange with the airline to provide oxygen. Different airlines have different rules and procedures, so it is best to contact the airline directly.
Preparing to fly checklist:

Respiratory infections, such as the flu or COVID-19, can increase your risk of becoming seriously ill if you have COPD. Vaccines can help lower your risk of getting seriously sick or hospitalisation. That is why getting all your recommended vaccines is an important part in the management of your COPD. Vaccination policies differ from country to country. Always follow the advice of your healthcare provider.
Following vaccinations may be recommended to you:
In addition to getting vaccinated, there are other precautions you can take to help prevent respiratory infections. These include washing your hands regularly, avoiding close contact with people who are sick, and considering wearing a mask in crowded places.
If you do get sick, your doctor might prescribe medicines such as antibiotics or antiviral drugs, depending on the cause of your infection. It is important to know that most respiratory infections are caused by viruses, not bacteria — and in those cases, antibiotics will not help.

To help avoid COPD flare-ups, it is important to reduce your exposure to things that irritate your lungs, such as smoke, strong smells, dust, chemical products, and fumes. Ventilate your home by opening up the windows regularly. When using household cleaning products, make sure to ventilate the room properly. If possible, choose unscented products or those with an Air Label certification.
If you’re exposed to dust, chemicals, or fumes at work, make sure to talk to your employer. Together, you can look for ways to make your work environment safer. This might include wearing a protective mask or, if necessary, adjusting your work setting to reduce exposure.
They moved to the term "healthy" air and it was accepted much more widely.

Living with a long-term health condition, like COPD, can affect your mood and mental wellbeing. It is completely normal to sometimes feel worried, frustrated, or sad.
However, if these feelings start to take over your daily life or affect your relationships, it is important to reach out to your healthcare provider. Anxiety and depression are quite common in people with COPD, but they often go unnoticed, both by yourself, your family or your healthcare provider.
Taking care of your mental health is just as important as looking after your lungs. Try to find meaningful connections with others—friends, family, or even people who also live with COPD. Explore ways to manage stress and make time for self-care, whether that is gentle exercise, relaxation, or doing something you enjoy.
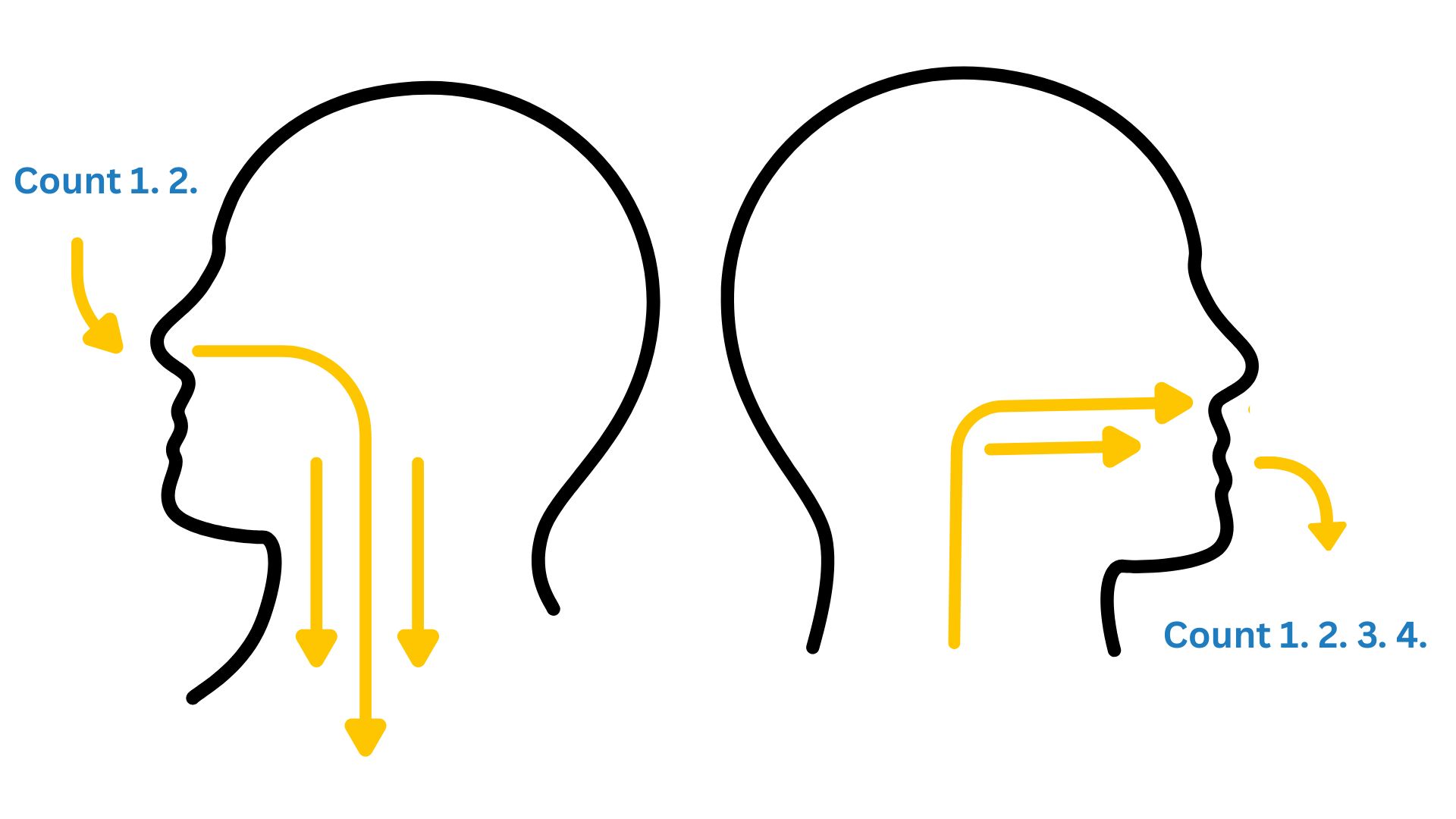
When you feel short of breath, it is a good idea to practise one of the following two breathing techniques: pursed-lip breathing or belly breathing, also called diaphragmatic breathing.
Pursed lip breathing is a breathing exercise that helps you slow your breathing and inhale and exhale more air. It reduces the number of breaths you take and keeps your airways open longer so you can be more physically active. To practise, breathe in gently through your nose, then breathe out slowly through your mouth with pursed lips. Try to make your exhale last about twice as long as your inhale. You can, for instance, count to two as you inhale and to four as you exhale.
Belly breathing (or diaphragmatic breathing) is a breathing technique that involves using the diaphragm muscle to take slow, deep breaths. The diaphragm is a large, dome-shaped muscle located at the base of the lungs. With this technique, you focus on using your diaphragm to help you breathe deeply. Most of the time, we only use part of our lungs. This exercise helps you use them fully and can make your breathing feel easier and more effective. Belly breathing can be a bit more difficult to perform than pursed-lip breathing, so it is best to learn it with guidance from a healthcare professional experienced in this technique.

If you have a cough that’s accompanied with a lot of phlegm, you may be taught a specific technique, called “autogenic drainage”, to help you clear your airways.

If you have COPD, you might have concerns about how your condition affects your relationships and intimacy. Just like any other physical activity, sex might make you cough or feel short of breath.
Feeling breathless or experiencing fatigue can impact your interest in sex. The fear of becoming breathless during intimacy might also cause you to become fearful of sex or less confident. In addition, some medications – whether for COPD or other medical conditions – can have an impact on your sexual health.
Although it might feel awkward, it is important to talk with your healthcare provider about your concerns. Challenges in the bedroom are very common for people living with lung conditions, so there is no need to feel embarrassed. Your doctor or nurse is used to these conversations and can offer helpful advice.
Tips for staying intimate

Caring for someone with COPD can be deeply rewarding, but it can also be challenging at times. It is important to remember that you do not have to do it all on your own. Take time to learn about the support options available to you, not just for daily tasks, but also for your own emotional well-being. Looking after someone with a long-term condition can be demanding, so sharing the responsibilities and talking about how you are feeling are essential, both for your loved one and for yourself.
Check out this resource for dedicated information for caregivers: https://www.nhlbi.nih.gov/education/copd-learn-more-breathe-better/copd-caregivers-toolkit.
This website does not provide medical advice.
The information, including but not limited to, text, graphics, images, and other material contained on this website is for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis, or treatment and/or medical treatment of a qualified physician or healthcare provider. EUFOREA is not a medical organisation and cannot provide specific medical advice to patients via the Internet and/or E-mail. All patients are encouraged to direct their specific questions to their personal physicians. EUFOREA presents this information to patients so that patients can understand and participate in their own medical care. EUFOREA strongly emphasises that the information contained on this website is not a substitute for thorough evaluation and treatment by a qualified healthcare provider.
© 2025 - EUFOREA - All rights reserved. All content on this portal, such as text, graphics, logos and images, is the property of EUFOREA. They may not be reproduced, copied, published, stored, modified or used in any form, online or offline, without prior written permission of EUFOREA.